Mesh Complications Patient Story 47
Lower Abdominal Pain, Pain with Intercourse, Vaginal Pain, Right Buttock Pain, and Urinary Incontinence following TVT Sling & Pelvisoft Graft with Sacrospinous Ligament Suspension
Mesh Complications: Lower abdominal pain, dyspareunia (painful intercourse), vaginal pain, urinary incontinence and right buttocks pain
Treatment: Laparoscopic removal of TVT sling and transvaginal removal of posterior repair mesh and sutures to sacrospinous ligament and repair of a rectocele via a posterior repair
The patient is a 37-year-old female who reports lower abdominal pain, vaginal pain and painful intercourse since her surgery. The patient originally had a LAVH (laparoscopic assisted vaginal hysterectomy), an anterior repair with Pelvisoft Graft (C.R. Bard), a posterior repair with Pelvisoft; attachment of the vaginal apex and posterior Pelvisoft to the sacrospinous ligament (SSL), and a TVT sling for stress urine leakage.
Just four months following her surgery she had a revision of the anterior vaginal wall graft. This was due to what the surgeon called “arcing” and laparoscopic adhesion removal for lower abdominal pain. The patient explained each time she attempted intercourse she had to go to the emergency room secondary to the pain. Because the surgery failed to relieve her pain, the patient drove to Atlanta from Savannah, GA for an evaluation by Drs. Miklos & Dr. Moore. Examination revealed pain at the urethra (consistent with the TVT sling placement), and along the posterior vaginal wall up to the right sacrospinous ligament (consistent with the posterior vaginal wall graft i.e. Pelvisoft and its attachment).
Dr. Miklos comment: Dr. Miklos is uncertain what the surgeon means by "arcing" or "arc-ing," but the pain the patient describes at the time of her evaluation by Dr. Miklos is essentially unchanged from the pain she felt during her second surgery four months after the initial procedures.
TVT sling – Complete Laparoscopic Removal
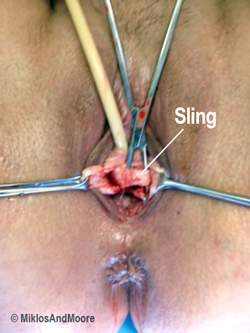
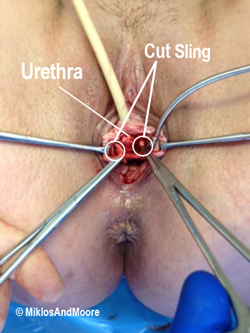
An informed consent was obtained, and the patient went to surgery. She agreed to have the TVT sling removed, and the posterior vaginal wall graft and its anchoring sutures removed at the sacrospinous ligament. The patient was taken to the operating room. An incision was made underneath the urethra to identify the sling (Figure 1).
The sling was identified and freed from the overlying urethra cut in the midline (Figure 2).
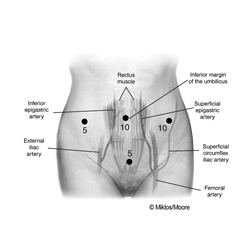
Dr. Miklos & Moore then approached the sling from above (i.e. laparoscopically) by making mini incisions in the abdomen (Figure 3).
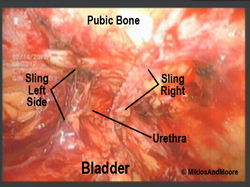
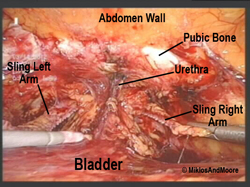
The space of retzius was entered (i.e. the space between the pubic bone and the bladder and urethra), and the sling identified (Figure 4).
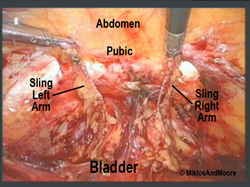
The sling was cut at the point of insertion at the abdominal wall (Figure 5) and the next picture shows the sling arms being pulled downward, so we could get a better view of the sling (Figure 6). The sling was then dissected away from the vagina side.
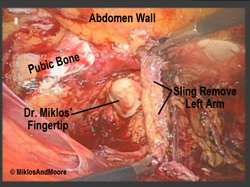
Dr. Miklos is meticulous at removing the entire sling out on each side of the urethra. Note; He started the surgery by doing the vaginal dissection. The sling goes through the ceiling of the vagina on each side of the urethra; the only way to remove the whole sling is to dissect all the way through the vaginal wall. Here, you can see Dr. Miklos‘ fingertip on the patient”s left side and the sling completely cut away from the urethra (Figure 7).
The same technique was employed on the patient’s right side. The total sling removed in two pieces seen on the operating room table (Figure 8).Pelvisoft and Sacrospinous suture removal.
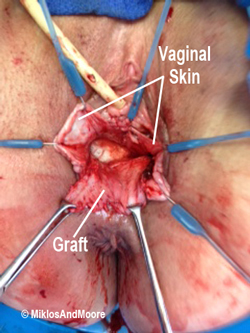
Upon completion of the TVT sling removal, Drs. Miklos & Moore approached the posterior vaginal wall graft (Pelvisoft) and anchoring sutures (lateral wall sutures i.e. levator ani muscles and apical or vault suture removal i.e. sacrospinous ligament removal). A horizontal and a vertical skin incision were made on the floor of the vagina (i.e. posterior vaginal wall), and the graft was dissected away from the overlying vaginal epithelium or skin (Figure 9).
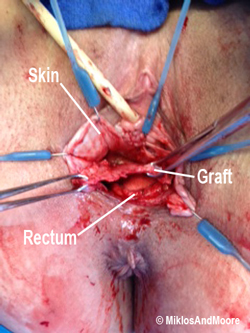
The graft was then meticulously dissected from away from the underlying rectal wall (Figure 10).
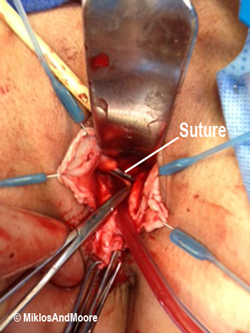
The sutures were removed at its lateral attachments (i.e. levator ani muscles). The levator ani muscles make up the right and left wall of the vagina. The sacrospinous ligament sutures on the patient’s right side are identified and are placed on tension in this illustration (Figure 11).
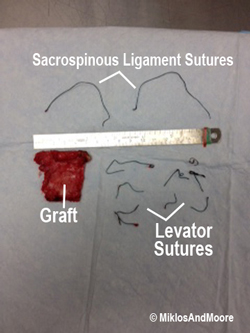
Removal of the posterior vaginal wall graft (i.e. Pelvisoft and the sutures that held it in place (Figure 12).