Mesh Complications Patient Story 24
Sacral Colpopexy Mesh Abscess
Mesh Complications: Vaginal and lower abdominal pain ten days after Laparoscopic Assisted Vaginal Hysterectomy (LAVH) and Sacral Colpopexy procedure
Treatment: Laparoscopic abscess evacuation and Y- mesh removal of sacral colpopexy mesh
The Patient is a 47-year-old female who initially had reconstructive vaginal surgery for uterine vaginal prolapse. She had a laparoscopic assisted vaginal hysterectomy for uterine prolapse, laparoscopic sacral colpopexy for vaginal vault prolapse, a laparoscopic paravaginal repair for a cystocele and a posterior repair for her rectocele. The patient's uterus had been prolapsing beyond the vaginal opening for more than a year before deciding to have the above surgery. The AMS Y-shaped mesh (see picture below) was used to do the sacral colpopexy. This mesh is a Type I macroporous polypropylene mesh (similar to Gynemesh) and is the standard mesh utilized in sacral colpopexies with the lowest rates of complications.
The patient consulted a pre-eminent urogynecologist in St. Louis who diagnosed her with IC (Interstitial Cystitis). He placed her on various medications (i.e. Elmiron). Her pain continued, and she was referred to a plastic surgeon. She received trigger point injections for the suspected diagnosis of nerve entrapment, which failed to relieve her pain. This plastic surgeon referred her to a fellow plastic surgeon that reportedly said, “They are all quacks.” Referring to gynecologists. The patient was then referred to a world-renowned urologist in St. Louis who specializes in female incontinence. The urologist did not believe the patient had IC. An ultrasound was ordered which revealed a thickening underneath the bladder. The urologist recommended the patient continue her care or follow-up with her urogynecologist.
Y-shaped mesh
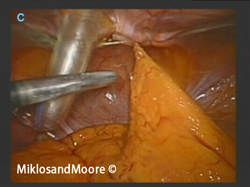
Using the previous incision sites Drs. Miklos and Moore approached the mesh removal laparoscopically.
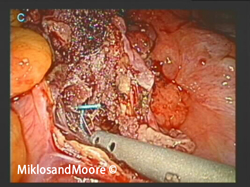
They entered the abdominal cavity to first remove adhesions (Photo 1).
They opened up the peritoneum covering the mesh at the level of the tailbone/sacrum. A green suture can be seen attaching the mesh to the sacral prominence (Photo 2).
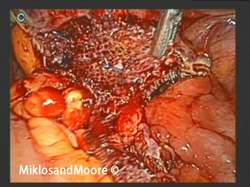
These sutures were individually removed as well as the sutures attaching the mesh to the vagina (Photo 3).
The mesh was completely removed from the sacrum and the vagina and the mesh is seen here still within the abdominal cavity (Photo 4) and outside the body (Photo 5).
Drs. Miklos and Moore Comment: The above complication was most likely due to an abscess or infection following the hysterectomy and could have occurred if mesh was or was not present. Rates of cuff abscesses following hysterectomies range from less than one %. If an abscess does occur and a mesh sacral colpopexy is completed at the time of hysterectomy the mesh may need to be removed in order to treat the infection.
Drs. Miklos and Moore recently published the worlds LARGEST series on Laparoscopic Mesh Sacral Colpopexy with over 400 patients utilizing the same type of mesh. The overall rates of complications were not significantly different whether a hysterectomy was completed at the time of the sacral colpopexy or not. In this series, they only had to remove one mesh due to an infection and it did occur in a patient that had a concomitant hysterectomy. It is important to note that this is the standard, accepted type of mesh that is used for sacral colpopexy and has been shown to be safe and effective in many studies. The recent FDA notification excluded this type of mesh placement from their announcement (meaning the warning was in regards to this type of mesh placement). Unfortunately, however, risks are associated with any type of surgery and the most important factor is having surgeons that recognize complications early and have the experience to treat such complications.
Click here to find out more about Sacralcolpopexy Mesh complications.
Click here for related patient stories