Mesh Complications Patient Story 44
Vaginal Pain, Painful Sex & Right Lower Abdominal Pain following Sacral Colpopexy with Mesh
Mesh Complications: Vaginal pain, bleeding, and vaginal drainage since surgery
Treatment: Laparoscopic removal of sacral colpopexy mesh and repair of chronic abscess and vaginal cuff secondary to the mesh
The patient is a 52- year-old woman whose original surgery was performed in Florida. She reports she had an immediate issue with mesh extruding (Mersilene Mesh, Ethicon) from her vagina. She reports she didn’t feel right (nor really has) for the first 18 months following her surgery. She had chronic vaginal drainage and discharge that was consistent with infection; she also had vaginal bleeding and pain.
In 2010, the patient underwent a mesh extrusion repair through the vagina; however, this did not work as she still had pain, discharge and bleeding and was told she still had a chronic mesh extrusion at the top of the vagina. She could also not have intercourse secondary to pain. She had no issues with the sling. She had no urinary leakage and overall the sling was doing well.
The patient decided to come to Atlanta (International Urogynecology Associates of Atlanta and of Beverly Hills) as her doctors told her the mesh would be very dangerous to remove and they would remove it through a large abdominal incision. This could result in a three to four day hospital stay and a six to eight week recovery period for the patient. The physicians of the International Urogynecology Associates approach these cases laparoscopically and have more experience than any center in the country with LAPAROSCOPIC MESH REMOVAL that can be performed in an outpatient type setting.
Dr. Moore comment: Very few surgeons in the world will remove the sacral colpopexy mesh because of the great difficulty associated with the procedure. Many surgeons will tell the patient that nothing can be done. Here at International Urogynecology Associates we can offer you the option of mesh removal not through a large incision, but through miniature incision (i.e. laparoscopically).
On physical exam, a large mesh extrusion was found at the top of the vagina with infectious type drainage (purulent and foul smelling). She had extreme pain on exam, as well. CT scan did not show evidence of an infection or abscess in the pelvis. The patient was taken to the operating room, and laparoscopy was performed. The mesh was identified.
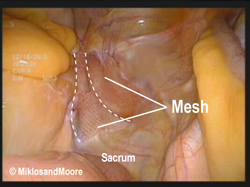
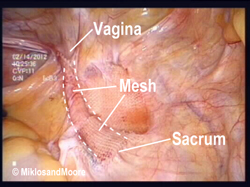
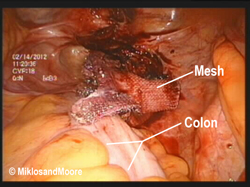
Picture 1 & 2- The previously placed mesh is identified in the pelvis. There did not appear to be any infection present in the upper pelvis (i.e. the upper portion of the mesh did not appear to be infected and had healed in place) and it did not appear that the infection had tracked its way up the mesh from where it was infected on the vaginal attachment.
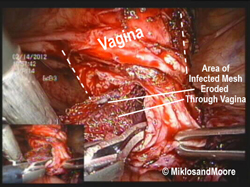
Picture 3- The peritoneum that covers the vagina and the mesh was incised. The mesh was very carefully dissected away and off of the vaginal apex where the chronic extrusion had occurred.
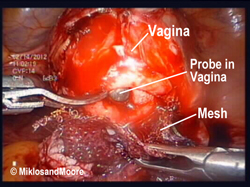
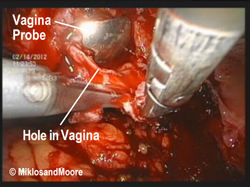
Picture 4 & 5- The mesh is taken off of the vagina (Picture 4). A walled-off cavity was located and was identified as the source of chronic infection and the area of mesh erosion through the vagina. The mesh was then completely dissected away from this area. Picture 5 indicated where the hole was at the top of the vagina (silver probe in the vagina can be seen).
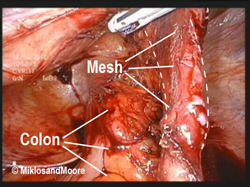
Picture 6 & 7 - The mesh was then dissected away from the bowel and up to the sacrum (Picture 6). It was removed from its attachment to the sacrum without complications, and the entire mesh was then removed and sent to pathology. The infected and scarred tissue at the top of the vagina was dissected and removed so that the top of the vagina could be closed anatomically with laparoscopic suture repair (Picture 7).
Picture 8 - Shows pelvis after complete removal of the mesh. A small drain was left through the top of the vagina for 24 hours to help prevent infection and the area was then covered with an anti-adhesive barrier to help prevent bleeding and post- operative adhesions.
Post-operatively she did very well. She travelled back home to Florida two days after surgery without complications. She no longer has discharge or bleeding and the pain is also resolving. She is very happy with her results and wished she had come to Atlanta much sooner for treatment.
Dr. Moore comment: Sacral colpopexy is a standard procedure for vaginal vault prolapse after hysterectomy and has the best cure rates in the literature. Please note there are risks associated with any surgery, whether mesh is used or not. Vaginal mesh exposure, although rare, does occur following sacral colpopexy. Infection can occur. This patient had an older type mesh that is rarely used anymore because the newer lighter weight meshes seem to have a lower rate of extrusions and infection. However, as in this case, if a complication does occur it should be recognized and treated in a timely fashion. If there is a chronic discharge or exposure the mesh should be removed. Many surgeons do not have this type of experience; therefore, the patient does no receive treatment, which can lead to further complications
Below is her testimonial just SIX weeks after her surgery:
“My infection started three years ago after my hysterectomy. The original surgeon placed the mesh after removing my uterus. My pain started instantly, but initially I thought the pain was normal pain related to having a major surgery. Three years later and multiple doctors later, I realized that the pain was not going away. Many doctors told me that the pain could not be resolved, that removing the mesh would be a complicated and difficult surgery. I didn't know where to go or who to call. I did some research on the Internet and came across Dr. Moore and Dr. Miklos' site. I read about their success with mesh removal and gave them a call. My initial conversation was with us, who was very informative and empathetic towards what I was going through. She told me that what I was experiencing should not be considered normal and that I needed to come see Dr. Moore. I did additional research on other doctors, just to make sure, but I kept coming back to Dr. Moore's site and my initial conversation with us. After meeting with Dr. Moore, I knew I was in the right place. He spent so much time with me and went over everything. I learned why this was happening to me, what he could do to help me and he told me what post surgery would be like; that I might not be 100% pain free as my body has had an infection in it for three years. I decided to have surgery with Dr. Moore and he was excellent! I feel so much better and I know that over time, this will all be a memory and not a daily reminder. Dr. Moore did what he said he would do and I feel like I have my quality of life back.”